- Home
- Cancer Type
A Comprehensive Guide To Oral Cavity Cancer – CancerMitr
ORAL CAVITY CANCER
The mouth, being the gateway to the digestive tract, is not only essential for consuming nourishment but also plays a fundamental role in effective communication. When the health of the mouth is compromised, it leaves individuals susceptible to a myriad of health issues, impacting their ability to eat, drink, and speak with ease. One particularly formidable threat is mouth cancer, a condition that instils a sense of unease, affecting three out of four individuals in middle-income countries. Cancer of the mouth is a nerve-racking condition that affects 3 out of 4 people living in middle-income countries.
Tobacco consumption is the leading cause of the disease. In India, tobacco and pan consumption is part of the culture in many parts of India and as many as 267 million adults are consumers.
India tops the global ranking in terms of the number of mouth cancer patients primarily due to the consumption of tobacco products like gutkha, dokha, kizami and beedi.
Bookmark this article to learn more about mouth cancer.
What is oral cavity cancer?
Mouth cancer or oral cavity cancer is a condition where cells in the mouth region undergo uncontrolled division and growth, leading to the formation of a deadly tumour. This type of cancer falls under the broader category of Head & Neck cancers, encompassing the nose (nasal cavity), paranasal sinus cavity, salivary glands, pharynx (throat), and larynx (voice box).
Statistics reveal that approximately 11 individuals per 100,000 will confront the diagnosis of oral cancer during their lifetime. Notably, men are more predisposed to developing oral cancer compared to women.
Also read: A Comprehensive Guide To Head and Neck Cancer – CancerMitr
Where does oral cavity cancer start?
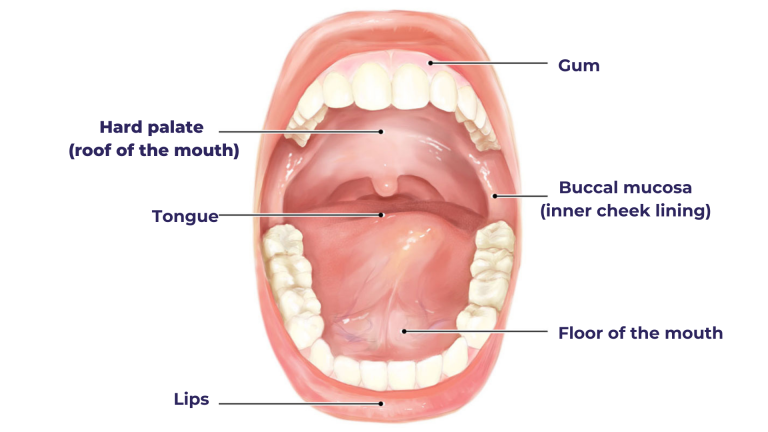
There are six crucial points in the human oral cavity: lips, roof of the mouth (hard palate), inner cheek lining (buccal mucosa), tongue, tonsils, and gums. A portion of the pharynx, the oropharynx, is also often regarded as part of the oral cavity. Cancer can form in any part of the oral cavity.
Most of the oral cavity cancers reported are squamous cell carcinoma. The squamous cells, characterized by their flat appearance akin to fish scales when observed under a microscope, undergo a transformation into cancerous entities due to alterations in their DNA. This pivotal shift prompts the abnormal growth and multiplication of cells.
Other cancers include lymphoma, adenoid cystic carcinoma (ACC), mucoepidermoid carcinoma, polymorphous low-grade adenocarcinoma, carcinoma ex-pleomorphic adenoma, mucosal melanoma, and sarcomas.
What are the risk factors of oral cavity cancer?
An oral cavity cancer risk factor is basically anything, biological, physical or chemical entity, that can increase the chances of developing oral cavity cancer. It is imperative for people to learn various risk factors linked to oral cavity cancer;
-
Tobacco: It is a universally known fact that tobacco can lead to cancers of the Head & Neck, lungs and blood. Tobacco chewing, as a habit, is prevalent in a country like India due to cultural reasons and therefore, the country tops the oral captivity cancer incidence list. Smoking or using tobacco increases the risk of certain cancers, especially those affecting the lips and cheeks. Smoked tobacco products include cigarettes, beedis, vape, kizami, dokha, pipe tobacco, and Mu'assel, and they are linked to cancers of the Head & Neck and lungs. Smokeless tobacco products include gutkha, snuff, naswar (popular in Afghanistan), iqmik (Alaskan smokeless tobacco), mava, dipping tobacco, and tambaku paan.
-
Alcohol: - Excess alcohol consumption increases the oral cavity and other Head & Neck cancers. A combination of smoking and drinking increases the risk even more.
-
Human papillomavirus (HPV) infection:- HPV is a group of over 150 types of viruses that cause a type of growth called papilloma or wart. Certain strains of HPV, notably HPV type 16 (HPV16), lead to cancer of the Head & Neck, oropharynx and tongue cancer.
-
Poor nutrition: The absence of fibre and plant-based food items in the diet significantly increases the risk of oral cavity cancer. Excess of a pro-inflammatory diet, rich in red meat and fried foods, can also increase the cancer risk.
-
UV radiation:- UV rays increase the risk of cancer in the lip region.
-
Genetic conditions:- Genetic conditions like Fanconi anaemia and Dyskeratosis congenita. Fanconi anaemia is characterized by early-onset blood problems, increasing the likelihood of leukaemia or myelodysplastic syndrome, along with a heightened susceptibility to mouth and throat cancers. Meanwhile, Dyskeratosis congenita manifests with aplastic anaemia, skin rashes, and abnormal nails, accompanied by a pronounced predisposition to head and neck cancers, particularly affecting the mouth and throat, occurring prematurely in individuals with the syndrome.
Showing signs of cancer? Click here to book a blood test.
What are the signs and symptoms of oral cavity cancer?
The signs and symptoms depend on the location of the cancer and may manifest itself as the following;
- Lump, bump or swelling in any part of the oral cavity
- Ulcer or sores in any part of the mouth that lasts longer than 15 days
- Unusual pain
- Difficulty chewing and swallowing
- Red or white patches in the oral cavity (that cannot be scrapped off or bleed easily)
- Numbness in any part of the oral cavity
- Unusual change in voice
- Weight loss
- Pain in ears
How is oral cavity cancer diagnosed?
The peculiarity of oral cavity cancer is that the signs and symptoms may be visible in their early stages because a person can literally feel and a second person can see it during the examination process. People should be aware that symptoms such as ulcers or sores that last longer than two weeks require immediate screening and intervention. Oral cancer diagnosis processes will be as follows;
- Physical examination: The dentist or an ENT specialist checks the oral cavity for various abnormalities. They pay attention to six crucial regions of the oral cavity: lips, hard palate, buccal mucosa, gums, tongue, and tonsils. They check for unusual lumps, bumps, bleeding, ulcers and more.
- Endoscopy: In some cases, the doctor may use a device called an endoscope, a small flexible camera equipped with a light, to check the various regions of the mouth.
- Biopsy: If anything suspicious is found in the cavity or pharyngeal (throat) region, the medical expert takes a sample for a lab test, a process called biopsy. It checks whether the cell is benign, precancerous or malignant.
- Imaging tests: Various imaging tests like CT, MRI, or PET-CT scans are done to check whether the tumour has metastasised or not.
What are the stages and grades of oral cavity cancer?
Oral cavity cancer staging follows the TNM staging process where the focus is on the tumour’s size (T), the number of lymph nodes (N) it invaded and whether it has metastasised (M) or not. Oral cavity cancer is categorised under 4 crucial stages;
-
Stage 0: It refers to a precancerous stage that needs immediate intervention to prevent malignancy.
-
Stage 1: The tumour is small and localised.
-
Stage 2: The tumour is smaller than 2 cm and not too deep.
-
Stage 3: The tumour is either bigger than 4 cm or it has invaded nearby lymph nodes.
-
Stage 4: The tumour has spread to nearby structures or to distant sites.
When it comes to the grading, like other cancers, mouth cancer also has three types of grades;
-
Grade 1 or low grade: Where the cancerous cells look almost similar to normal cells.
-
Grade 2 or intermediate grade: Where the cancerous cells look somewhat different to normal cells.
-
Grade 3 or high grade: The cancerous cells look extremely different from the normal cells.
If the grade cannot be assessed, then the cancer is categorised as Gx.
Don’t avoid cancer treatment!
CancerMitr provides a holistic treatment plan to tackle all cancer-related challenges, including side effects management. Check out our website for more details.
How is oral cavity cancer treated?
The treatment of oral cavity cancer depends on the stage and grade of the disease. The cancer treatment plan is designed in such a manner that the disease is removed from the human body while making sure that the person gets to live a normal life. The “cancer cure” is a scenario where the tumour is completely removed from the body without leaving behind a trace. Various treatment processes that can help cure, if not control, the disease are as follows;
- Surgery:
It is the most important and effective form of treatment where the tumour, along with some healthy tissue, is removed. When it comes to big tumours, radical procedures may be needed. For example, the complete removal of a jawbone or a portion of the tongue or buccal mucosa. If cancer has spread to neck lymph nodes or if there’s a high risk, a neck dissection may be recommended to remove the affected tissue. It clears cancer cells and helps determine further treatment needs. Different types of surgeries are as follows;
- Tumour resection: It is the surgical removal of a tumour or abnormal growth from the body.
- Mohs micrographic surgery: It is a precise surgical technique meant for removing skin cancer, involving successive layers of tissue examination under a microscope to ensure complete tumour removal.
- Glossectomy: It is the surgical removal of all or part of the tongue.
- Mandibulectomy: It is the surgical removal of a portion or the entirety of the mandible (lower jawbone).
- Maxillectomy: It is the surgical removal of a portion or the entirety of the maxilla (upper jawbone).
- Trans-oral robotic surgery (TORS): It is a minimally invasive surgical procedure using robotic technology for accessing and operating within the oral cavity and throat through the mouth.
- Laryngectomy: It is the surgical removal of the larynx (voice box).
- Tracheostomy: It is the surgical creation of an opening (stoma) in the trachea (windpipe) to facilitate breathing.
- Reconstruction surgery: Medical experts may perform reconstructive surgery to restore a certain portion of the face. Surgeons may use skin, muscle, or bone grafts from elsewhere to rebuild your mouth. Dental implants can also replace natural teeth.
- Chemotherapy:
It is a treatment process where powerful drugs are used to target and destroy cancerous cells in the oral cavity region and other parts of the human body. Chemotherapy is given either before surgery to reduce the size of the tumour (neoadjuvant chemotherapy) or after surgery to destroy the cancer cells in the human body (adjuvant chemotherapy). A type of chemotherapy where drugs that target proteins ( e.g., epidermal growth factor receptor (EGFR) in cancer cells is called targeted drug therapy.
- Radiation therapy:
It is a type of cancer treatment where powerful X-rays and protons are used to target and destroy cancerous cells. It is delivered from either outside the body (called external beam radiation) or from inside the body through radioactive seeds and wires (brachytherapy). Radiation is also given either before surgery (neoadjuvant radiation therapy) or after surgery (adjuvant surgery).
- Immunotherapy:
It is a type of treatment where the body uses its immune system to target and destroy harmful tumours. However, it is important to note immunotherapy is usually recommended only for advanced cases of cancer.
Have you been suffering from an ulcer that has lasted for more than 15 days?
Book a test now!
What are the different side effects of oral cavity cancer?
The cancer treatment process involves the target and destruction of human body cells that go rogue and unleash terror. The process may also affect the normal human cells, leading to side effects that may affect the person’s quality of life.
The biggest concern around Head & Neck cancer, especially mouth cancer, is how badly it may affect the person’s quality of life. Any radical structural changes due to treatment processes like surgery or radiation affect the person’s ability to eat or speak and sometimes breathe normally. Some people may not be able to move their jaws or neck normally without additional support.
Other side effects of cancer treatment include;
– Lymphedema: After surgery or radiation therapy, the lymph nodes may not be able to drain themselves properly, leading to the building of fluid and lymphedema.
– Hair loss: Chemotherapy may lead to hair loss, a condition called alopecia.
– Nausea and vomiting: Chemotherapy may lead to constant feelings of nausea or vomiting due to various reasons, including sensitivity towards various smells and tastes.
– Chemo brain: Cancer treatment may lead to issues linked to a person’s ability to think or concentrate.
– Taste changes or tasteless: Chemotherapy may lead to thick saliva or a sharp metallic taste in one’s mouth, leading to tastelessness.
– Sore throat or mouth ulcers: Due to the way in which the chemotherapy affects the normal cells, a person may suffer from severe sore throat or mouth ulcers that affect their ability to chew.
– Difficulty opening the mouth: Radiation therapy can damage nerves in the facial muscles, affecting the person’s ability to open their mouth.
– Dry mouth: Radiation therapy may damage the salivary glands, leading to thick saliva or dry mouth.
– Osteoradionecrosis: Radiation therapy may damage the blood supply to the facial bones.
– Neutropenia: It is a commonly reported side effect experienced by oral cancer patients undergoing treatment processes like chemotherapy or radiation therapy. It is a condition that is characterised by a decrease in the number of neutrophils in the human body.
What are the different supportive therapies for oral cavity cancer?
Cancer treatment does not stop with just chemotherapy or radiation therapy. While these treatment processes aim to target and destroy cancerous cells, it is important to enhance the quality of life of the patient. Supportive therapies aim to make life as smooth as possible for the patient. Reconstruction surgery is an important form of supportive therapy provided to all patients who have undergone surgery. It can restore some of the facial features and the ability to speak and eat normally. Other than that, patients undergo the following supportive therapies;
- Jaw motion exercises:
It is recommended for those patients who experience pain while chewing, pain (in the ear, face, jaw, and neck), difficulty opening the mouth, speaking, or swallowing, locking of jaw joints and headaches. A specialist assists in the movement of the jaw. Mouth cancer patients cancer wear prostheses, especially those who experience severe facial or palatal changes or defects due to the progress of cancer or due to treatment processes like surgery or radiation therapy.
- Speech therapy and sign language:
They are integral components of rehabilitation for patients facing challenges in verbal communication post-treatment. Experienced professionals provide guidance and support to individuals, focusing on techniques to enhance the coordination and strength of jaw muscles, as well as improving mobility in the neck and shoulders for effective speech production.
- Olfactory rehabilitation:
It is essential for patients undergoing treatment for head and neck cancer, as radiation therapy in proximity to the nose can lead to a loss of smell. Specialized medical professionals in this field employ strategies aimed at enhancing nasal airflow, such as nasal airflow-inducing manoeuvres, to aid in the restoration of olfactory function.
- Complete decongestive therapy (CDT):
CDT, or complex decongestive therapy, integrates skin care, manual lymphatic drainage, exercise, and compression. It’s best performed by a doctor specializing in lymphedema or a CLT. They’ll teach you the techniques for self-care at home and advise on frequency.
- High dose vitamin C (HDIVC):
Cancer treatment processes like chemotherapy may leave the person vulnerable to infections as the result of low blood count. High-dose intravenous vitamin C (HDIVC) promotes healing and bodily immunity along with the formation of free radicals and has a pro-oxidant effect.
- Colony-stimulating factors:
To deal with neutropenia, patients may have to undergo treatment with medications called colony-stimulating factors (CSF) or white blood cell growth factors.
- Ice therapy:
Ice chips help manage mouth sores, dry mouth, and change of taste to an extent.
- Aromatherapy:
It may help in dealing with nausea sensations.
- Pain management:
It is a critical aspect of rehabilitation for patients experiencing discomfort in various areas, such as the head, neck, jaw, or body. Rehabilitation methods encompass a range of modalities, including therapeutic exercises, aquatic therapy, electric stimulation, acupuncture, acupressure, massages, and appropriate medication tailored to address individual needs and alleviate pain effectively.
- Nutrition consult:
Patients may suffer from various nutrient deficiencies during cancer treatment due to side effects like loss of appetite due to nausea and vomiting. A specialised onco nutritionist can help in tailoring a suitable diet.
What are various products oral cavity cancer patients can try for a better quality of life?
- Maxillofacial prosthesis: Restores facial appearance and function after surgery or trauma.
- Therabite: Helps regain jaw movement and function after oral surgery or injury.
- Cervical collar: Supports and immobilizes the neck to aid in healing after injury or surgery.
- Dentures: Replace missing teeth to restore chewing ability and enhance appearance.
- Skin care products: Maintain healthy skin, prevent ageing, and treat various skin conditions.
- Compression sleeves: Improve blood circulation and reduce swelling in limbs.
- Sugar-free lemon drops, gum, or mints: Help manage dry mouth and promote saliva production.
- Nicotine lozenges or gums: Aid in smoking cessation by reducing cravings for nicotine.
- Cold caps: Minimize hair loss during chemotherapy by cooling the scalp.
- Heating Pad: Relieves muscle aches, pains, and stiffness through heat therapy.
- Oral Tinctures: Deliver medication or supplements orally for quick absorption.
- Lip Balm: Hydrates and protects lips from dryness and cracking.
- Post-Surgical Chin Strap: Supports the chin and aids in recovery after chin surgery.
- Immunity Booster Juices: Provide nutrients and antioxidants to strengthen the immune system.
- Curcumin liquid: Harnesses the anti-inflammatory properties of curcumin for health benefits.
- Bedroom Humidifier: Maintains optimal humidity levels to alleviate dryness and congestion.
- Cinnamon or Citrus Lozenges: Soothe sore throat and freshen your breath.
- Aloe Vera Mouth Wash: Promotes oral hygiene and soothes gum irritation.
- Walking stick (if required): Provides stability and support while walking, especially for those with mobility issues.
- Parallel press system: Assists in upper body strength training and rehabilitation exercises.
- Bite pads: Aid in dental procedures by providing a stable surface for biting.
- Squeeze bottle: Dispenses liquids with precision, often used for wound care or hydration.
- Mouth key: Assists in opening the mouth during medical procedures or dental work.
- Mould: Used to create custom-fitted dental appliances or prosthetics.
- Ryle’s tube set-up: Administers nutrition or medication directly into the stomach for patients unable to swallow.
- Glass bottle/ Thermos flask/ Copper flask: Store and carry liquids, keeping them at desired temperatures.
- Acupressure twisters: Stimulate pressure points on the hands or feet for pain relief and relaxation.
What lifestyle changes should people with oral cavity cancer make?
– Smoking and using tobacco increase the risk of oral cavity cancer. Quitting smoking and avoiding all forms of tobacco is crucial for reducing the risk of developing or worsening oral cancer.
– Along with that, limiting alcohol intake or abstaining altogether can help lower the risk of developing the disease.
– A diet high in fruits and vegetables provides essential vitamins, minerals, and antioxidants that support overall health and may help reduce the risk of oral cancer.
– Brushing teeth regularly, flossing, and using mouthwash can help maintain oral health and reduce the risk of oral cavity cancer.
– Using lip balm with sunscreen and wearing hats or other protective clothing can help prevent damage from UV radiation.
– Regular dental check-ups allow for early detection of any abnormalities in the mouth, including signs of oral cavity cancer. Early detection greatly improves treatment outcomes.
– Staying hydrated helps maintain oral health by promoting saliva production, which can help protect the mouth from harmful bacteria and reduce the risk of oral cavity cancer.
– Chronic stress can weaken the immune system and potentially contribute to the development or progression of cancer. Engaging in relaxation techniques such as meditation, deep breathing, or yoga can help manage stress levels.
– Regular physical activity supports overall health and well-being, which can help reduce the risk of various types of cancer, including oral cavity cancer.
Coping with a cancer diagnosis can be challenging, both emotionally and physically. Seeking support from healthcare professionals, counsellors, or support groups can provide valuable assistance and guidance throughout the treatment process.
In conclusion,
Oral cavity cancer is still a major global health concern that affects people of all ages and socioeconomic backgrounds. Even while receiving a diagnosis could seem overwhelming, patients’ quality of life and prognosis can be greatly enhanced by early detection and rapid treatment. We can all work to lessen the incidence of oral cavity cancer by increasing awareness and encouraging preventive actions like routine dental checkups, quitting smoking, and leading healthy lives.

