- Home
Challenging The Standard Of Care: Novel Strategies For Advanced Cancer Treatment
– By Cancer Patient Lab, Medium.com
John Doe has cancer. He is discussing his treatment options with his oncologist. The oncologist explains a treatment plan that is based on the current standard of care: a carefully tried and tested treatment backed by evidence from robust clinical trials. He also explains the importance of hitting cancer hard from the start, so the plan is to administer the maximum dose John can tolerate killing as many of the tumour cells as possible, and when the treatment stops working, they will discuss other options.
It’s impossible to know how well the treatment will work for John until he actually takes it, but the doctor reassures him that the data from the clinical trials are good and that a statistically significant percentage of patients survive up to twelve months before the treatment fails and they need a new option.
John leaves the clinic with a heavy feeling. The uncertainty around his treatment options and the doctor’s language make him feel like a statistic. What happens when his tumour resists treatment? What if he runs out of options?
Although John is a fictional patient, his story is representative of many people whose cancer is treated based on standardized treatment plans. The problem with these plans is that they are based on population averages, yet everyone’s tumour is different. So why are they all treated the same way? And why subject patients to the rollercoaster of hope with a new treatment, followed by anxiety and disappointment when it fails, only to start that cycle over and over again until there are no more options?
Bob Gatenby, MD, Moffitt Cancer Center, Co-Director, Center of Excellence for Evolutionary Therapy, and Department Chair, of Diagnostic Imaging, has been pondering these questions and advocating for novel strategies for advanced cancer treatment. His approach is based on evolutionary and game theory and experimental models, with a more nuanced approach to cancer treatment, which takes into consideration the uniqueness of each patient’s cancer and its response to drugs, beyond the strategy of taking a single drug at maximum tolerated dose until it fails.
The strategies include combining therapies, low doses, sequencing treatments, and using mathematical simulation models for maximum impact. This is in contrast with the predominant treatment strategy where a patient is given the maximum drug dose they can tolerate until their tumors become resistant to it.
Dr. Gatenby and his colleagues see limitations in the clinical gold standard of evidence — double-blind randomized trials, which they argue have some benefits but also some drawbacks. These drawbacks are more apparent as we move to personalized cancer care with targeted molecular therapies.
“>”>The Scientific Hypothesis
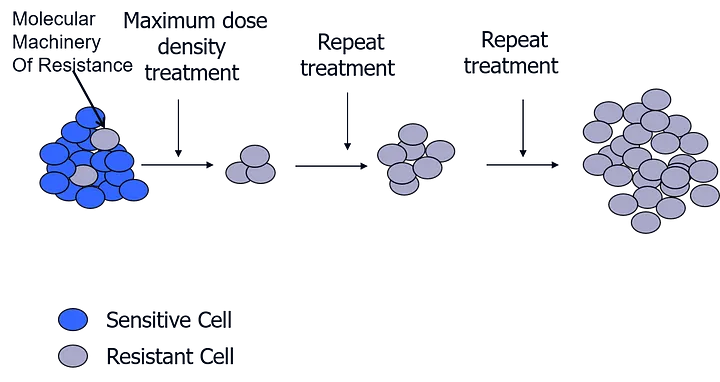
Dr. Gatenby’s team’s method is based on the understanding that any tumor comprises a mixed population of cancerous cells. All these cells want to do is to keep multiplying. As the tumor environment has limited resources, these multiple cells compete with each other. Cancer cells also develop the ability to change and adapt to their environment to keep multiplying. So, if a tumor is subjected to a treatment, some of the cells in the mixed population are selected because they are resistant to treatment. However, this can come at a cost.
Adaptive therapy leverages the cost of developing resistance. Since the sensitive cells do not have the burden of the resistance mechanisms that the resistant cells have, the sensitive cells have an advantage. When treatment is paused, sensitive cells outcompete the resistant cells. The strategy is to use the sensitive cells that you can control, to control the resistant cells that you cannot control. In other words, you change the dynamics within a tumor to improve the outcomes of treatment.
“>”>The Treatment Strategy
Here are several key underlying principles of a treatment strategy that can control the evolution of an advanced cancer:
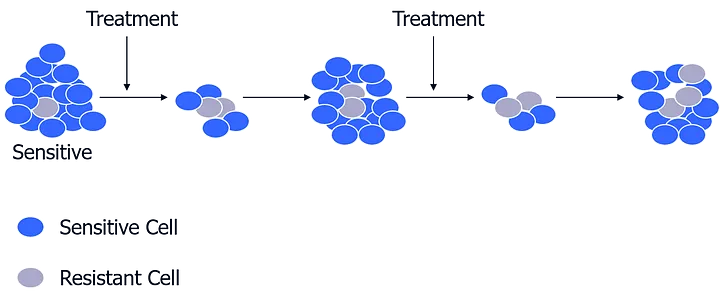
- Apply a low dose: Hit the tumours with enough treatment to perturb their system, but not so much to kill all the sensitive cells, thereby leaving the environment free for the resistant cells to proliferate. The resistant cells can be controlled by keeping enough of the sensitive cells around.
- Apply treatment combinations (first strike, second strike): Lacking magic bullets, metastatic cancers can be kept under control through a strategic combination of pretty good bullets. None of these bullets could by themselves cure the cancer, but the combination could.
- Sequence treatments (not a combination cocktail): If you have a combination cocktail, especially as a first strike, you’re applying the therapy to the largest possible population. The heterogeneity of the cancer cells is such that almost certainly, you will find tumor cells that will be resistant to the combination. It is better to hit the cancer with therapies in sequence, as each knocks the population down and can drive it to extinction.
- Use mathematical models as a guide: Having a hypothesis and a simulation of what should happen based on evolutionary theory helps in understanding why and enables insights from much smaller trial cohorts.
“>”>Does it work in real life?
Dr. Gatenby shared a study using an androgen-suppressing drug (Abiraterone) in this adaptive therapy on-off mode, monitoring disease progression through PSA (prostate-specific antigen — a measure of disease progression) tests. Seventeen (17) patients completed the trial and were compared to 16 demographically similar patients who had the same 50% PSA decline with the initial Abiraterone dose, but who then got standard-of-care dosing.
The difference in median time to progression was 14.3 months on the standard of care, compared to 33.5 months on adaptive therapy. Overall survival in the standard-of-care cohort was 30.4 months vs. 58.5 months in the adaptive therapy group. 4 of the 17 adaptive therapy patients are still alive and on treatment, over six years since their treatment began. The patients on the adaptive therapy did not get treatment about half of the time, which resulted in a cost reduction of an average of $70,000 per patient per year.
To apply this strategy in real life, we asked Dr. Gatenby to give his off-the-cuff thoughts on the case of advanced cancer patient Brian McCloskey, who was taking Abiraterone, the drug that Dr. Gatenby used in his study. Dr. Gatenby felt that because Brian currently has a low tumour volume that he is a candidate for an attempt at extinction, to hit his cancer with a ladder of three different drugs to successively knock down the population, with the hope that it could be nudged down the vortex.
Over to you
Do you have any feedback on Dr. Gatenby’s principles for treatment strategy?
This adaptive strategy seems intuitive, yet it’s not widely practiced. What are the barriers or objections to it?
Disclaimer: The article was originally published in the Medium.
“>Think you have cancer? Seeking treatment option?”>
CancerMitr provides holistic care for all cancer-related challenges, from discovery to recovery. Inspired by loss but driven by purpose, we focus on the patient’s journey with a comprehensive care plan which covers diagnosis, treatment, and support therapies. Visit our website for additional information on the many packages we provide.

